Personal experiences of birth trauma

What the research had to say
COPE research undertaken with 1,899 consumers, revealed that 37 per cent of individuals identified challenges around the time of birth. This included managing a traumatic birth.
Source: Centre of Perinatal Excellence (2022) 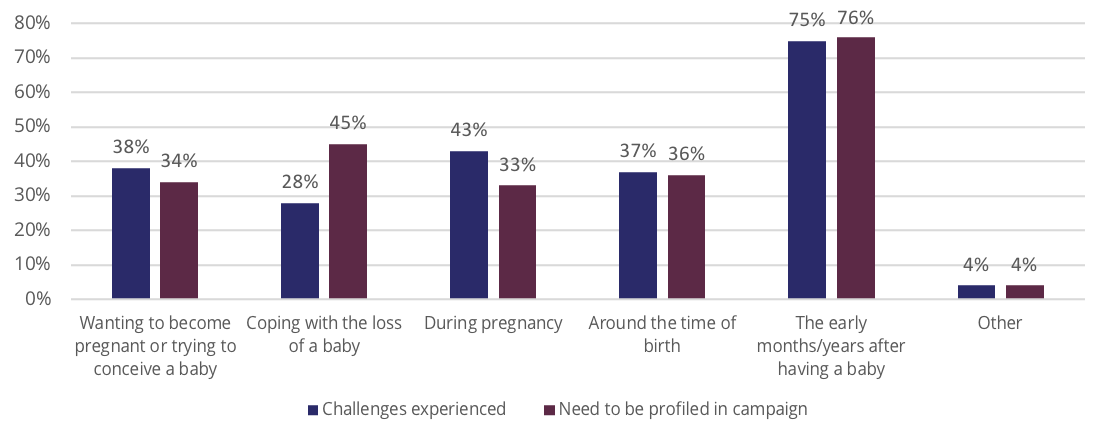
Below are the key themes identified pertaining to personal experiences of challenges around the time of birth. These themes informed the development of The Truth campaign.
Birth trauma
Respondents described high levels of physical and psychological trauma which could impact both the mother and father/partner.
“Feeling shock and disbelief, that my body could go from completely healthy and capable, to being a shadow of myself.
When focusing on the psychological themes particularly, this was associated with perceptions surrounding the poor delivery of care they received around the time of birth – by health professionals and the health system.
Powerful language was used to describe these experiences – including feeling “powerless” “violated” “belittled” “bullied” and “betrayed” particularly by health professionals who were supposed to be caring for them.
“Not understanding my rights, not understanding ‘hospital jargon’ and being treated like a statistic not a mother; all lead to me being bullied into procedures I didn’t want to have.”
“My husband was traumatised too. He was referring to the doctor as a butcher.”
The longer-term impacts of birth trauma were also reflected in subsequent pregnancies whereby women elected to have inductions or planned C-sections as a result of fear and to avoid re-experiencing trauma.
“If I’m honest I haven’t recovered yet and three years on I don’t think I will ever recover.”
Lack of continuity of care around the time of birth
Here, women described being ‘passed around the system’ and being ‘treated like a number’.
“Inadequate staffing with midwives, fragmented management of my on ward care and dismissive attitude of a number (though not all) midwives which I was deeply hurt by as it was my first child and I was inexperienced and dependent on their support.”
Treatment by health professionals following birth
They also noted that when they attempted to speak about their experiences, they were minimised by others, in particular health professionals (and in some instances family and friends).
“I do not feel anyone at the hospital who has an impact has listened, acknowledged my experiences and anxiety and provided appropriate care. Instead I feel invalidated, belittled, insignificant, like I’m being dramatic and an inconvenience.”
“Unsupportive midwives at the hospital comparing me to other mothers in the rooms next door who ‘had a baby yesterday and are walking around the ward.”
“Despite showing signs of depression I was ignored or dismissed by GP and family. I had to find my own way out.”
“Also, nurses and lactation consultants at hospitals can be mean, make us feel belittled, they all give conflicting advice, some are plain rude when we are our most vulnerable. You’d expect much more sensibility from professionals that chose to work in this field.”
For many, the only outcome that seemed to matter was the health of the baby.
“I was told to be grateful that I had a child. As if I wasn’t unbelievably grateful that we had survived almost dying. I was told ‘at least the baby is OK. As if I didn’t matter.’”
“We need more focus on the mother from health professionals: GPs, OBGYN, MCHN, Physiotherapists… we go to so many appointments and they are all focused on the baby. The 6-week check-up for the mother I believe should be much earlier as the first 4 weeks are horrible and there’s no support, and should happen again, not just once.”
Lack of opportunity to debrief
The lack of opportunity to debrief following a traumatic birth was a common theme. This made it more difficult for respondents to process and come to terms with what had happened.
“Absolutely zero discussion of what happened during the birth. Everyone forgets it straight away and moves on. No one talks about birth in society either so you’re left to deal with it on your own.”
“Medical staff should be taught to debrief women after their birth – no matter the experience.”
“Being in the public service, I’ve never had a ‘debrief’ on what happened during birth. It’s crazy when you think it’s probably the biggest thing you’ll ever go through, and yet you have no debrief on what happened. it puts so much pressure on you as a woman, to have to cope and ‘get on with it’”
Impacts of birth trauma long-lasting
Once again the impacts could be long-lasting: increasing anxiety and depression, PTSD, and affecting their ability to attach to their baby. Respondents also described strong fear and/or avoidance of subsequent pregnancies.
“Traumatising. I will never have a baby again.”
“Although I have come to terms with happened and I can now talk about it, it is something which changed me as a person and the trauma and pain will never be forgotten.”
Additional challenges in the early postnatal period
In the context of having a traumatic birth, other factors such as breastfeeding, sleep-deprivation, exhaustion and coping with a new baby added to the burden experienced by new parents.
Respondents described being uneducated and unprepared about what to expect in the days and weeks following birth. This was largely attributed to the fact that antenatal classes focus on the lead-up to, and the actual birth itself, with little focus on the early postnatal period.
Emotional vulnerability in the postnatal period was also made worse by perceived lack of support, particularly around breastfeeding. Many also described that receiving conflicting advice undermined parents’ confidence in their new role and their confidence in professionals and the system.